A Discussion with Dr. Catalona: Managing Continence & Other Side Effects After a Radical Prostatectomy
 One of the most feared side effects of total prostate removal (radical prostatectomy) for treatment of prostate cancer is urinary incontinence, but that fear far outweighs the reality.
One of the most feared side effects of total prostate removal (radical prostatectomy) for treatment of prostate cancer is urinary incontinence, but that fear far outweighs the reality.
“Permanent incontinence after a radical prostatectomy occurs infrequently with an experienced surgeon,” Dr. Catalona said.
He explained that it is important to know the anatomy in the area of the operation and to be gentle so as to prevent as much trauma and bleeding as possible.
Bleeding makes it hard for a surgeon to see what he’s doing. When a surgeon has a good view, he can be precise, meticulous and dissect in exactly the right place.
“Most important is not to injure the muscle fibers of the external sphincter,” Dr. Catalona said. “I call it the ‘no touch technique’. Do your best to leave them the way God made them.”
“The fear far outweighs the reality.”
He explained that temporary incontinence is usually (although not always) a component of post surgery recovery. Bladder control starts improving soon after the catheter is removed, but it could take six to 18 months for the complete return of continence in some patients. After that time period, little improvement is expected.
While incontinence seems to have several definitions, Dr. Catalona uses only one: “If men have to wear any kind of protection at all, they are incontinent.”
Using that definition, five and a half percent of his patients have a very mild incontinence 18 months after surgery and one and a half percent have severe incontinence. Age figures strongly into these outcomes and so does the fact that some men go into the surgery with previous incontinence.
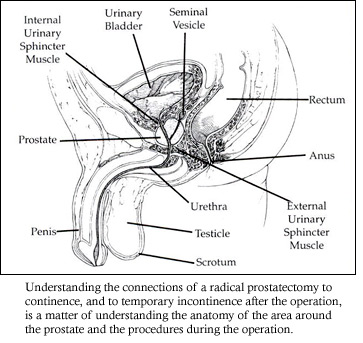
Understanding the connection of a radical prostatectomy to continence, and to the temporary incontinence after the operation, is a matter of understanding the anatomy of the area around the prostate and the procedures during the operation.
The prostate is a plum sized gland that lies below the bladder and inbetween the bladder and the urethra. The urethra, which carries the urine out the body, starts at the bladder, runs through the prostate and then continues through the penis.
“When a surgeon cuts out the prostate, a gap is created between the bladder and the urethra. The bladder must be pulled down and the urethra pulled up so that the two can be surgically reconnected,” Dr. Catalona explained.
“Frequent urination is normal after a radical prostatectomy.”
The larger the prostate the bigger the gap and sometimes the more difficult to reconnect the bladder and the urethra. In addition, the internal sphincter muscle, the muscle that involuntarily controls bladder output, is removed with the prostate.
After the operation, men who had three layers for holding back urine – the internal sphincter muscle, the prostate lobes pressing against each other, and an external sphincter muscle – have only one, the external sphincter.
“The external sphincter can do all the necessary work to hold in the urine, but it has to be strong. That’s why the Kegel exercises, both before and after surgery, are so important,” Dr. Catalona said.
He explained why procedures during the surgical removal of the prostate cause temporary incontinence and how time and the healing process usually fix the situation.
The bladder and the urethra must be connected to each other but if they were just sewn together, postoperative swelling of the tisues would close the opening for the urine to pass through. Temporarily, they need a stent to preserve the opening, and that stent is the catheter.
The bladder is always being emptied by the catheter. The bladder isn’t holding urine and therefore doesn’t expand as long as the catheter is in place. When the catheter is removed, the bladder is a shrunken version of itself.
“Over weeks and months, the bladder expands again and, most often, returns to normal size and normal function,” Dr. Catalona said.
Bladder training after catheter removal
Dr. Catalona knows that men are anxious to have the catheter removed, but most often, they leave the hospital with a catheter in place and it remains for one to two weeks, rarely more. The time frame for removing the catheter depends upon how nicely the urethra and bladder come together. If it’s with little tension and little stretching, the catheter can be removed sooner.
Also, when the bladder is exposed during the surgery, it takes some physical blows and it swells, just as other parts of your body swell when they take a hit.
“Frequent urination is normal after a radical prostatectomy,” Dr. Catalona said. “The main cause is that the bladder wall is swollen and thickened and irritable. Normally, the bladder wall is thin and very elastic and maintains a low pressure until it has stored 8 to 10 ounces of urine. After surgery, the swollen bladder does not store much urine at a low pressure. As soon as it starts to fill, the pressure goes up and the patient feels the need to urinate. In the great majority of cases, this gradually improves with time, but it can take more than a year in some cases.”
Other consequences occur too.
“You create surgical planes or in lay terms, cuts, and as those cuts heal, it’s possible they create scars,” Dr. Catalona said.
Later in the healing process, those scars can cause difficulties for the bladder because they make it difficult for the bladder to expand as it should. The scars increase the time it takes for the bladder to expand and therefore increase the time to return to continence.
“Also, sometimes after surgery, the patient can get a stricture at the point where the urethra and bladder are connected. Then, after the catheter is removed, the already irritated bladder is trying to force out the urine through a pinpoint,” Dr. Catalona said.
Often, symptoms are the worst at night.
“After surgery, some fluid that is retained in the lower half of your body during the day gets redistributed at night and is excreted by the kidneys at night,” Dr. Catalona explained.
Eventually, most damage to the bladder and the urethra heal, but it takes time and the improvement in continence is gradual, with complete recovery taking from six to 18 months.
Incontinence after prostate cancer treatment & surgery
“The most common cause of incontinence after a radical prostatectomy is a weak external sphincter muscle,” Dr. Catalona said. “The surgeon has to try his best not to injure it and to preserve its length.
“Most important is to protect muscle fibers of external sphincter.”
 A recent study at Memorial Sloan Kettering connected the length of the sphincter before surgery with how quickly continence returned after surgery.
A recent study at Memorial Sloan Kettering connected the length of the sphincter before surgery with how quickly continence returned after surgery.
The external sphincter muscle squeezes the urethra, enabling it to retain the urine until the sphincter releases its hold. Its action is both involuntary and voluntary. The effectiveness of the sphincter is a combination of length and strength. The longer it is, the more efficient it is. The stronger it is, the more effective it is.
Patients can not control how long their sphincter muscle is, but they can contribute to how strong it is by doing Kegel exercises as recommended by their doctors both before and after surgery.
“Kegel exercises are so important.”
“But men aren’t always as compliant as they should be,” Dr. Catalona said.
Also, he added that it doesn’t help to do Kegel exercises improperly. Sometimes, men are told to squeeze their buttocks together and that instruction is incorrect.
In describing how to do Kegel exercises, Dr. Catalona recommends to his patients that they imagine they are in the bathroom urinating and someone opens the door. They would cut off their stream and hold it for a second or two.
After surgery and after removal of the catheter, he suggests doing this exercise in sets of 10, four times a day – before breakfast, lunch, dinner and bedtime.
When patients do urinate, he tells them to stop in midstream once or twice. Then they will know they are exercising the correct muscle.
“If as men begin to regain continence, they leak in the evening, it’s caused by fatigue,” Dr. Catalona said. “Sometimes it happens after drinking a glass of wine and that’s because the alcohol has caused the muscle to relax.”
Overexercising does not help. In fact, it can slow down the healing and strengthening process.
“The idea that if 10 are good, 100 are better and a 1000 even better doesn’t work. The sphincter muscle is recuperating after surgery and it will get fatigued if the exercises are repeated too many times,” Dr. Catalona said.
Age is a definite factor in return of continence, most likely because, as with other muscles, the condition of the sphincter muscle deteriorates with age.
Also, Dr. Catalona said that about 30% of his patients over 50 years old have some version of bladder instability or stress incontinence before the operation.
“Men can not expect to have better control of their bladders after the operation than they did before,” he said.
Few options are available for men who are mildly incontinent, but in outcome studies measuring function and bother, the small percentage of men in this category don’t report high levels of concern.
For the one and one-half percent of men who have severe incontinence, correction is possible with the surgical implant of an artifical urinary sphincter or a urethral sling procedure.
“The operations do work,” Dr. Catalona said. “Most patients who have the procedure improve almost immediately. I’m not sure why more men with the severe incontinence don’t request it. Perhaps, they have had enough of surgery and are relunctant to go through the experience again.”
Most important for patients to know is that the very nature of a radical prostatectomy causes a temporary incontinence, but in most cases, bladder control starts to improve after the catheter is removed and continence returns within six to 18 months.
Proper surgical training and experience are key factors in the success of regaining continence after RRP surgery. Dr. Catalona does extensive follow-up on patients, and as part of that follow-up, men are asked if they would be willing to share their experiences with other patients.







