The PSA Story: It’s A Lot More Than a PSA Score
Misop Han, M.D.; Peter H. Gann, M.D., Sc.D.; William J. Catalona, M.D. prepared a paper on PSA and Screening for Prostate Cancer for the journal Medical Clinics of North America. This article is a portion of that paper revised by Cecilia Lacks, PhD, for QUEST readers
An annual PSA test as well as a digital rectal exam are, at present, the best diagnostic tools for the detection of prostate cancer.
But PSA, prostate specific antigen, is about a lot more than one PSA score.
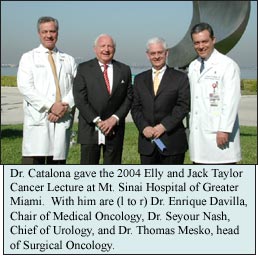
After the initial results of a large community screening study initiated in 1989 were analyzed, Dr. Catalona first reported in the New England Journal of Medicine in 1991 that PSA could be used as a first-line screening test for prostate cancer. Other studies on PSA soon followed.
The new information has shown that a total PSA score (tPSA) was only the beginning for detecting prostate cancer. Then came discoveries of PSA variations and studies that showed these variations could be helpful in clarifying and confirming the information and diagnoses suggested by tPSA.
What Is Prostate-Specific Antigen (PSA)?
PSA stands for prostate specific antigen. An antigen is a protein, in this case produced by the prostate gland. PSA plays a role in making semen a liquid when it leaves the body.
PSA forms are measured in serum or plasma, taken in blood tests. (In QUEST, the word blood is used instead of serum or plasma.)
For the most part, PSA stays in the prostate gland and is in the bloodstream in barely measurable amounts. But when something is going wrong in the prostate, PSA is over-produced in the gland and leaks into the bloodstream. Even then, amounts are very, very small.
Ng/mL
PSA scores are reported in nanograms per milliliter (ng/mL). For example, a doctor or a patient might say the PSA is 2.6, but understood is 2.6 ng/mL. (In QUEST, the PSA numbe is written without the ng/mL.)
To give an idea of how small this measurement is: A nanogram is one-billionth of a gram. A gram is equivalent to 1/28 ounce. A milliliter is equal to 1/1000 liter. A liter is slightly larger than a quart.
Measurements of one billionth of a gram and 1/1000 of 28 ounces are extraordinarily minute. The difficulty in interpreting some of the variations of PSA tests results from the difficulty in accurately measuring these miniscule concentrations.
Why PSA Testing
At present, the measurement of PSA in the blood is widely used for the screening and early detection of prostate cancer.
However, because other medical conditions can also cause high PSA levels, a prostate biopsy is needed to confirm a diagnosis of cancer.
Also, PSA is used frequently in determining the need for a repeat biopsy in men with previously negative prostate biopsy.
In addition, a rising PSA is significantly associated with an increased risk of prostate cancer.
Most recent studies show that 35-45% of man with a PSA between 4 and 10, will have detectable prostate cancer, and the great majority of the tumors, if left untreated, have a high probability of causing death or disability during a patient’s lifetime.
These studies also show that at least 20% of men with PSA levels 2.6-4 have readily detectable prostate cancer.
Improving Accuracy
The measurement of PSA, what is called the total PSA (tPSA), is not as accurate a detector of prostate cancer as doctors or patients would hope because PSA levels can also be elevated with benign conditions such as BPH (benign prostatic hyperplasia), prostatitis, recent ejaculation and minor trauma to the prostate by digital rectal examination, catheterization, or urinary retention.
Substantial efforts have been made to find more specific ways to do PSA-based screening, ways that would allow doctors to know the difference between PSA elevated from benign conditions and PSA elevated from prostate cancer – and without unnecessary biopsies.
The methods most studied include: percent free PSA, complex PSA, pro-PSA, PSA “velocity”, PSA “density”, age-specific PSA reference ranges, and hK2.
Free and Complexed PSA
PSA exists in the blood serum in two general forms: free-floating PSA and PSA complexed (attached) to proteins. When a man gets back his PSA result, it is the total measurable PSA, which is the combination of fPSA and cPSA.
Separately, the free PSA test measures the amount of PSA not bound to another protein in the blood and then that value is compared to the amount of bound PSA.
Prostate cancer is more likely to be present if the ratio of free PSA to total PSA is less than 15%; therefore, low free PSA values are more likely to be associated with prostate cancer than high free PSA values.
These compared measurements of free PSA and complexed PSA improve the ability to tell whether a rising PSA is from cancer or benign prostatic disease.
The percent of fPSA in blood is increased in men with BPH because the inner portion (“transition zone”) of the prostate, where BPH predominantly occurs, contains elevated levels of certain forms of fPSA that leak into the bloodstream but aren’t naturally there otherwise.
Pro-PSA
Prostate cancer, on the other hand, develops predominantly within the peripheral zone of the prostate gland.
Studies from this area reveal another form of PSA, called proPSA, which is elevated in cancerous prostate tissue. For reasons still unknown, pro-PSA accumulates in the tumor.
Pro-PSA has many forms. One, [-2]pro-PSA, has received the most clinical attention because it has been the primary form found in tumor samples.
The ratio of pro-PSA to free PSA has been shown in preliminary studies to be a most effective predictor of cancer in patients with total PSA levels in the 2.6-4 range and works almost as well in the 4 to 10 range.
If these studies are verified, pro-PSA levels might be preferable to free or complexed PSA as a clinical marker for cancer.
With greater acceptance and use of lower PSA cutoffs, more men will be advised to have biopsies and then pro-PSA markers could serve to eliminate unnecessary biopsies.
Although studies are showing the value of knowing the various concentrations of pro-PSA in the blood, a commercial test is not available yet.
Improving Accuracy in PSA Testing Using:
percent free PSA
complex PSA
pro-PSA
PSA “velocity”
PSA “density”
Age-specific PSA
HK2
Complexed PSA
Typically between 70 & 90% of the PSA in blood is in the cPSA form, with the remainder being fPSA.
Studies reporting the clinical value of complexed PSA are conflicting. Some show that cPSA measurements are more helpful in predicting the presence or absence of cancer than total PSA and more accurate than percent fPSA when total PSA ranges below 6 ng/mL.
Other studies show that fPSA and cPSA both provide more information than total PSA, but the measure of either without knowing the total PSA is not more helpful. Perhaps, with more information from studies, using the cPSA percent will be helpful in selecting men for repeat biopsies.
A limitation of screening with cPSA alone is that it doesn’t indicate the total PSA level, which can vary considerably for any value of cPSA. In clinical practice, the results of using cPSA alone are similar to those obtained using tPSA alone.
By itself, complexed PSA does not provide information as helpful as the free-to-total PSA ratio (i.e., percent PSA).
PSA Velocity
PSA velocity measures the rate of change of PSA as a function of time.
An increase in the PSA level of 0.75 ng/mL per year has been reported to be suspicious for prostate cancer.
Only a small percentage (1% to 2%) of men with very low PSA levels have rapid PSA rises. However, these men have the most aggressive cancers and the most to lose from delayed detection.
An important limitation of PSA velocity is that it takes time and multiple measurements to determine whether a biopsy is necessary. Also, a man might have cancer, BPH, and prostatitis, all at the same time, which could produce confusing PSA patterns.
PSA density
The prostate-specific antigen density (PSAD) test compares the PSA value to the size of the prostate gland.
A PSA density cutoff in the range of 0.10 would be an acceptable sensitivity for cancer detection but, at the present, a commonly used cutoff of 0.15 is probably too high and misses cancer in many patients.
Also, a disadvantage of using PSA density measurements is that they require transrectal ultrasonography to accurately determine the prostate volume.
Age-Specific PSA reference ranges
Age-specific PSA reference ranges refer to using different PSA cutoffs for recommending prostate biopsy. The most commonly used age-specific PSA reference ranges are 2.5 for men in their 40’s, 3.5 for 50’s 4.5 for 60’s and 6.5 for over 70.
These age-specific reference ranges do not work because using them would miss or delay the detection of prostate cancer in 20% of men in their 60’s and in 60% of men in their 70’s.
PSA and Biopsy
Results from several of our studies (Han, Gann, and Catalona) have shown that a higher proportion of patients are diagnosed with organ-confined cancer when lower PSA cutoffs are used.
Also, the progression-free survival rates (cure rates) correlate with the PSA level at the time of diagnosis.
These studies, and others, also suggest that cancer can be detected earlier without materially over-detecting potentially harmless prostate cancers.
A concern about using lower PSA cutoffs is whether lower cutoffs are more likely to detect harmless cancers. For many cancers, it is not difficult to determine whether they are potentially dangerous. These are the high-grade, large-volume tumors.
It is more difficult – in fact, impossible – to state which cancers are clinically harmless. However, a screening strategy designed to detect only high-volume, high-grade cancer would compromise treatment outcomes.
The goal of screening should be to detect cancers with favorable prognostic features, i.e., low PSA, low-volume, intermediate Gleason grade cancers that are organ-confined. The hope is that information from these PSA variations will assist in their identification.







