Prostate Cancer – PSA Testing & Treatments
Dr. Catalona Responds to Stories and Studies About Use of PSA Testing and Treatments for Prostate Cancer
In the following Questions and Answers, Dr. Catalona responds to questions he hears most often
regarding PSA testing, early detection, and prostate cancer treatment.
In light of so many confusing and contradictory messages in recent media coverage, Dr. Catalona
is concerned that men know what the research is showing so that they are able to make informed decisions.
Q: Why is so much attention being paid to PSA testing now?
A: After a 10-year study on PSA testing, my colleagues and I published) our findings that recommended a lowering of the PSA threshold for a biopsy from 4 to 2.5. (New England Journal of Medicine, 2003)
This recommendation brought immediate media and research attention to PSA and its use in early detection of prostate cancer.
Most recently, an article by Dr. Ian Thompson reported that 15% of men with PSA values less than 4 and a normal prostate examination had cancer detected with a prostate biopsy.
I had previously reported this finding for men with PSA levels from 2.5 to 4 and recommended using a lower (2.5) cutoff to detect most of these cancers.
Also, an article by Dr. Thomas Stamey of Stanford University reported that PSA is no longer a marker for prostate cancer but is related only to the size of the prostate gland. Dr. Stamey criticized our findings.
The media coverage and medical interest in his comments have caused men to question the use of PSA in screening for prostate cancer and to question the appropriateness of a radical prostatectomy for treatment of many patients with prostate cancer.
Dr. Stameys comments, along with news stories about unnecessary biopsies, costs of screening, and possible over treatment or unnecessary treatment of prostate cancer have created more confusion and controversy than the information deserves.
I am concerned that these stories could cause men to put off the life-saving detection provided by an annual PSA test and the timely treatment after a prostate cancer diagnosis.
Q: In general, what does your research show?
A: My research and the research of my colleagues show the most effective and acceptable treatment for prostate cancer is to get rid of the tumor at a very early stage before it has a chance to spread.
The risk of unnecessary treatment is low when good clinical judgment is exercised.
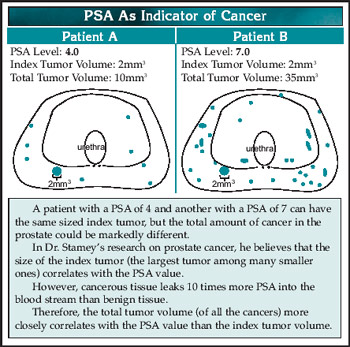
Also, its important to know that prostate cancer is not like many other cancers in that we talk about a tumor, but early prostate cancer is more like clusters of cells forming microscopic tumorlets that can be in many different places in the prostate. It is almost never one single tumor.
Since advanced prostate cancer has no known cure and there are no means to prevent prostate cancer, the only hope is to detect it early and treat it effectively.
Because prostate cancer usually produces no symptoms until it is too late, it is necessary to screen for and detect it when it is curable.
A recent study shows that radical prostatectomy reduces the chances for metastasis (spreading of the cancer to other parts of the body) and death from prostate cancer as compared with watchful waiting.
Q: What do you recommend for prostate cancer screening?
A: I recommend an annual PSA and digital rectal examination beginning at age 40, or earlier in men with a family history of early age-at-onset prostate cancer.
A PSA level of 0.6 to 0.7 or less in men 40 to 50 years old is evidence of a healthy prostate gland.
I recommend monitoring PSA velocity, the rate at which a PSA rises – if and when it does begin to rise.
A 12 core biopsy of the prostate with a local anesthetic should take place if the digital rectal exam is suspicious, if the PSA is higher than 2.5, or if a PSA velocity is higher than 0.75 in a year.
In addition, I recommend using PSA velocity, PSA density, percent free PSA, percent complexed PSA, and measurement of androgen levels to determine the need for repeat biopsies.
All the tests and measurements listed above are explained on my website (www.drcatalona.com) in language for the general reader.
Q: Why do some reports say that PSA tests are misleading and result in unnecessary treatments?
Why do you say these reports, like the ones from Dr. Stamey, are wrong?
A: To some extent, PSA has become a victim of its own success. With widespread screening, tumors are smaller at the time of diagnosis now than in the past.
Some years ago, as is the case with Dr. Stameys research, doctors made a connection between the index tumor (the largest single tumor of many tumors they found in the removed prostate) and the PSA level in the blood.
But now, weve learned how to use the PSA test to detect cancers before a large index tumor can develop when the patient has cancer in the form of multiple small tumorlets and thats the life-saving nature of PSA findings.
Dr. Stamey says that the lower PSAs dont reflect the existence of any substantial cancer. He is not correct. Even at the lowest PSA levels, the level of PSA in the blood correlates with likelihood of finding prostate cancer on biopsy.
Even when the largest tumor (index) is small, if multiple tumors or tumorlets are present, they can produce slight increases in the PSA level in the blood.
If the only purpose of PSA testing were to detect a large index tumor, the test would not be of any use because the detection of a large index tumor meant a high probability of death from prostate cancer no matter what the treatment.
It has been estimated that PSA screening detects prostate cancers 5 to 13 years sooner than they would be detected without PSA testing. Just because the tumors are smaller upon this detection doesnt mean that they do not have or cannot acquire a lethal potential.
In fact, our research shows that the great majority of PSA-detected tumors have the characteristics of clinically important cancers, meaning that given more time, they will develop into cancers that will spread and will be life-threatening.
Fortunately, now, most cancers we find are organ confined, and treatment by a skilled doctor provides a good chance of no recurrence in a large majority of patients.
Q: Can you be more specific about your findings that support the usefulness of PSA testing?
A: My PSA Study enrolled 36,000 men for screening and lasted for 12 years. After a few years, it became apparent that nearly half of the men whose PSA was in the 2.5 to 4 range progressed to PSA levels above 4 within four years.
In nearly one-third of these men with rapidly rising PSA, the cancer had spread to the margins of the prostate or beyond by the time the PSA had reached 4. Fewer than 10% had tumors meeting the established criteria for possibly harmless cancers; meaning 90% did have potentially dangerous cancers.
(Although I also use the established criteria for possibly harmless prostate cancers – .0.3 to 0.5 cubic centimeters, organ confined, and a Gleason score of 6 or less I do not believe that anyone can say which cancers are truly harmless and which will in time change to high-grade, deadly cancers.)
Some reports critical of our recommendations say the 2.5 cutoff means more unnecessary biopsies, but, in fact, in most cases it simply means that the biopsy is performed at an earlier time.
The current American Cancer Society and the 2004 National Comprehensive Cancer Center Network guidelines also recommend consideration of a biopsy for a PSA above 2.5.
Furthermore, our studies have demonstrated that a high PSA velocity during the year before diagnosis of cancer is strongly associated with the risk for prostate cancer death.
Our results indicate that PSA trends are more important than any single PSA value in assessing the risk for life-threatening prostate cancer.
(For those interested in reading more technical information, journal articles are available on my website: www.drcatalona.com)
Q: What is the history of your involvement with PSA testing?
A: My colleagues and I report on information from 3,477 patients whom I have treated with a radical prostatectomy from 1983 to 2003.
PSA began as a detection tool for prostate cancer in 1991, when I discovered, in a follow-up study of my patients, that measuring PSA in the bloodstream could be used as a first-line screening test for prostate cancer.
Before this discovery, the digital rectal exam was the principal way prostate cancer was diagnosed. But, for the most part, by the time a tumor was felt, the disease had progressed too far for successful treatment. Even with treatment, many patients died of prostate cancer. It is the second leading cause of death from cancer in US men.
Fairly soon, the PSA blood test became the accepted method for detecting prostate cancer in the United States and internationally.
At first, in the PSA era, more men were diagnosed with prostate cancer. And the questions started arising in regards to PSA testing: If were going to find more men with prostate cancer and were going to do more biopsies, how are we going to pay for them and how do we know that earlier detection prevents deaths?
What did happen in the PSA era is that the death rate from prostate cancer turned around. Now 80% of diagnosed patients have cancer that is completely contained within the prostate gland.
Some critics say that PSA testing found patients who didnt need treatment and thats why the death rate decreased so drastically. My research, and that of my colleagues, shows this criticism is not valid.
(In addition to the research findings I described above, see published on my website: www.drcatalona.com)
Meanwhile, weve found many forms of PSA in the bloodstream. And these different forms are telling us much more about prostate cancer detection and diagnosis in specific individuals than the initial PSA test indicated.
Q: What Do You Tell People About PSA Testing?
A: I say, without reservation, that PSA testing detects most prostate cancers when they can be cured with skilled medical treatment. Other medical diagnostic tests do not do as well as the PSA test.
The PSA blood test does better in diagnosing prostate cancer than the mammogram does for breast cancer, and yet PSA remains controversial.
If there were no effective treatment for prostate cancer, early detection would not be important. But studies are showing that patients treated with a radical prostatectomy have fewer deaths and less spreading of the cancer compared to those in a watchful waiting program.
The most effective and acceptable treatment is to get rid of the prostate cancer at a very early stage before it has a chance to spread. Nobody should want to go back to the pre-PSA screening era when most prostate cancers grew out of control before they were detected.
Every man hopes to be cured with primary treatment and no additional therapy. No one wants to hear about long-term hormonal therapy, chemotherapy, or harsh experimental treatments. The risk of unnecessary treatment is low when good clinical judgment is used.
PSA testing, with all its variations, is improving every year. Until we have more information on the genetic influences for prostate cancer, the PSA test will be the first line technique for early detection and, when required, successful treatment of prostate cancer.