Dr. Catalona Discusses Nerve-Sparing Surgery
 Defining a nerve-sparing radical prostatectomy is easy: During the surgical removal of the prostate gland, an attempt is made to spare the two cavernous nerve sheaths (lying slightly underneath and to the sides of the gland) that produce erections.
Defining a nerve-sparing radical prostatectomy is easy: During the surgical removal of the prostate gland, an attempt is made to spare the two cavernous nerve sheaths (lying slightly underneath and to the sides of the gland) that produce erections.
Completing the nerve-sparing surgery successfully and deciding who should have it are much more difficult than defining it.
“Early diagnosis is so important.”
Dr. William Catalona, who has performed more nerve-sparing radical prostatectomies (3381) than anyone in the United States, said that with an experienced surgeon and effective pre-operative testing, nerve-sparing surgery has a high success rate.
His definition of success is not easy on himself or other surgeons, but is reassuring for patients.
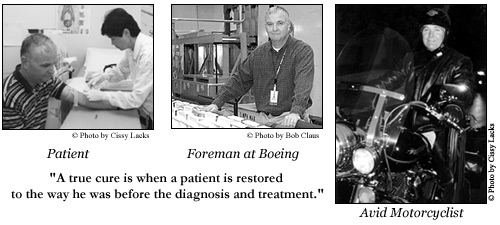
“A true cure is when a patient is restored to the way he was before the diagnosis and treatment of his prostate cancer,” Dr. Catalona said.
“It’s not really a cure if a man is impotent and incontinent after surgery.” (Continence is not connected directly to nerve-sparing surgery. That topic will be covered in a future issue of QUEST.)
Because diagnostic techniques are discovering prostate cancer in earlier stages and in middle-aged men, Dr. Catalona said that his goal of returning a man to the way he was before the operation – cancer free, continent and potent – is increasingly attainable.
Nerve-sparing surgery is not for everyone, and patients who were impotent before surgery are not candidates for nerve-sparing surgery.
Dr. Catalona’s patients make their decisions before the surgery to direct him to attempt the procedure but after reviewing findings of pre-operative biopsy results, rectal exams, scans, and PSA levels.
“The first priority is to remove all the cancer,” Dr. Catalona said. “If tests show that the cancer has spread beyond the margin of the prostate gland, the cavernous nerves must be removed because we know cancer cells travel along the spaces surrounding those nerves.”
One concern of nerve-sparing surgery is the risk of not removing all the cancer.
“Theoretically, because nerve-sparing surgery preserves the soft tissues around the prostate, there is a higher risk for cancer recurrence,” Dr. Catalona said.
That theoretical concern is seldom the outcome in Dr. Catalona’s patients.
In studies of his patients, Dr. Catalona found that the recurrence rate for cancer is actually less in men who have had nerve-sparing surgery. He believes that finding is a consequence of performing the surgery on men who have the most favorable conditions for the operation in the first place, and he emphasizes that early diagnosis is extraordinarily helpful in obtaining good results.
“My patients want to know that their cancer is removed. Next, in my experience, men are concerned about continence. And then they want to be potent. I, too, am concerned first and foremost that all the cancer is removed,” he said.
During the operation, the decision for sparing the nerves is influenced by how easily and cleanly the prostate can be freed from the neurovascular bundles.
To explain the procedure in lay terms, Dr. Catalona compares the nerve-sparing operation to the lifting of a boxcar off a set of railroad tracks.
“In nerve-sparing surgery, doctors try to gently lift the ‘box car’ off the railroad tracks without damaging the ‘tracks’. If the cancer is detected early, then the prostate can more likely be removed without disturbing the nerves,” he said.
“But at the best, the nerves usually get bruised and stretched somewhat during the operation or require suturing to control bleeding, which is why it can take 3 to 6 months for erections to begin to return after surgery. With time, up to 36 months after surgery, the nerves regenerate, so it’s very important to detect the cancer while still on the inside of the prostate because after it grows out into the nerves, they can’t be spared.”
Another comparison he made was to peeling the shell off a hardboiled egg. “Sometimes, the shell peels right off the egg and sometimes you have to pick it off,” he said.
When the prostate gland lifts beautifully off the neurovascular bundles, the surgeon knows that the nerve-sparing part of the operation has gone well. When it sticks, then some of the nerve fibers must be sacrificed and the outcome is more uncertain.
Nerve sparing surgery is not about injuring or removing a single nerve. The cavernous nerve “tracks” are like cables and their bundles include nerves, arteries, veins and lymphatic channels.
If the prostate is stuck a little, the surgeon can remove the gland and just some of the cable. Then, only some of the nerve fibers will be lost. If the gland is stuck a lot, then a good portion of the nerve fibers must be removed or damaged.
“First priority…remove all the cancer.”
The nerve fibers carry impulses that tell the blood to flow into the blood vessels and initiate the erection. If too many nerve fibers are damaged, not enough impulses are sent to get enough blood flow to the penis. Whereas loss of erections is connected to removal of the nerve bundles, sex drive and orgasm are not.
“The idea is to gently peel the prostate off the nerves without stretching, bruising, cauterizing or hurting the nerve fibers,” Catalona said.
Damage could occur for various reasons. One would be if the surgeon needed to pull and tug on the prostate as it’s lifted. Another would be if the nerves were cut by accident, more likely to occur with a surgeon who does this operation infrequently. Or they might have to be removed because of additional evidence revealed during surgery.
Also, cauterizing to stop bleeding creates a heat that could damage the nerves. Dr. Catalona said that he does not cauterize near the nerves because of this potential damage.
With laparoscopic removal of the prostate, it is more difficult to separate the prostate gland from the nerves without using a harmonic scalpel that cuts by heat.
Putting in stitches to stop bleeding can also cause damage to the nerve fibers.
 Prostatectomies are described as being performed retropubic (RRP) or perineal, describing from what direction or area the surgeon approaches the prostate gland. Dr. Catalona performs RRPs because he feels that the cavernous nerves can be more readily spared. He explained that from the retropubic approach, the prostate gland is lifted up off the nerves. From the perineal approach, the gland must be pulled down between the nerves.
Prostatectomies are described as being performed retropubic (RRP) or perineal, describing from what direction or area the surgeon approaches the prostate gland. Dr. Catalona performs RRPs because he feels that the cavernous nerves can be more readily spared. He explained that from the retropubic approach, the prostate gland is lifted up off the nerves. From the perineal approach, the gland must be pulled down between the nerves.
The skill, experience and record of the surgeon are major factors in the successful outcome of nerve sparing surgery, but a patient’s anatomy is also a consideration.
“Gently peel the prostate off the nerves.”
Nerve-sparing surgery is harder to do when the prostate is large, according to Dr. Catalona. Other concerns are scarring around the prostate, which can be a result of multiple biopsies, previous prostate infections or prior surgery to treat an enlarged prostate.
Also, hormonal therapy before surgery can complicate the nerve-sparing component of the operation by producing scarring around the prostate gland.
While it is best to have treatment as soon as convenient, it becomes another issue of how long to wait is reasonable if it is necessary to delay. Dr. Catalona said that patients, with appropriate diagnostic test results, can choose, if necessary, to wait three or four months.
“Hormonal therapy may be indicated for longer delays, but that choice has its risks,” he said. “It doesn’t always ruin things, but it does make the nerve-sparing procedure more difficult.”
“Age is a factor in recovering potency.”
Proscar is the mildest treatment and causes the least scarring. Stronger forms, like Lupron or Zoladex, cause more scarring.
At the annual meeting of the American Urological Association in May of this year, Dr. Catalona presented results from a series of his 3,032 consecutive patients who had a radical retropubic prostatectomy (RRP), most with some form of nerve-sparing surgery.
“Age is a definite factor in recovering potency,” Dr. Catalona said. “And better results are achieved in young men with early-stage disease. That’s why early diagnosis is so important.”
For instance, during the PSA screening era (1992-2002), in men under 50 for whom he performed bilateral nerve-sparing RRPs, 94% were potent after 18 months. In ages 50-59, 86% regained potency. In those 60-69, 72% regained potency and in those over 70, 52% regained potency.
Not many surgeons specialize in prostatectomies to the exclusion of other surgeries, but experience is a key factor in the success of nerve-sparing surgery and also continence after RRP surgery.
Dr. Catalona has research assistants whose full-time jobs are to follow-up on patients regarding potency, continence and cancer. As part of the follow-up, men are asked if they would be willing to share their experiences with other patients. For those who agree, contact information is given to prospective patients.
While Dr. Catalona knows that such follow-up is not possible for most surgeons, he does believe that a patient should be able to ask his surgeon to provide a list of 10 men who would be willing to talk to him about the outcomes of their prostate operations.











