Dr. Catalona’s Recommendations for Early Prostate Cancer Detection

SEER Cancer, the authoritative source for cancer statistics in the US, estimates that about 7 out of 8 men will never be diagnosed with prostate cancer during their lifetime, and nearly 90% who receive the
diagnosis never suffer or die from it. Men without prostate cancer and those with indolent cancer tend to have persistently low PSA levels unless they develop significant benign enlargement (called BPH for “benign prostatic hyperplasia”), prostatic inflammation (called “prostatitis”), are genetically high PSA producers, or take long bicycle rides sitting on a hard saddle which can bruise an enlarged prostate. In contrast, those with aggressive prostate cancers have more rapidly rising PSA levels (called the “PSA doubling time,” “PSA velocity,” or “PSA growth rate”). The prostate cancer early detection guideline panels of several professional organizations would like to limit the amount of unnecessary testing that occurs in the population and, therefore, recommend longer intervals between PSA screenings. However, determining the steepness of the PSA growth function requires multiple PSA measurements at shorter PSA intervals.
Dr. Catalona believes that to reduce suffering and death from prostate cancer, screening intervals should not be too lengthy; annual screening intervals offer the best opportunity to reduce suffering and death from prostate cancer.
Cancer cell growth is an “exponential function,” going from one cancer cell to two to four, etc. For exponential functions such as PSA growth, the steepness of the PSA growth curve depends in part on the absolute value of the PSA at the start of the measurement period, i.e., the higher the baseline PSA at the beginning of measuring, the faster the PSA increases. Thus, the PSA velocity is lower in men with low baseline PSA levels. However, except for some rare types of prostate cancers (i.e., neuroendocrine or undifferentiated cancers) that do not produce much PSA (and for which an expert prostate exam might be informative), serial PSA testing of the population stratifies men into two essentially different risk groups (1) a large group whose PSA levels are not rising rapidly and (2) a small group whose levels are rising. To reduce as much as possible cancer-related suffering and death, doctors should monitor men
with rising PSA levels more intensively to diagnose a life-threatening cancer early and treat it effectively. For this reason, Dr. Catalona believes long re-testing intervals for a man with a single low PSA level may be “throwing away the baby with the bathwater.”

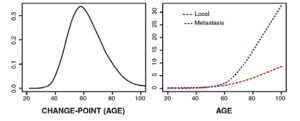
Supporting this opinion is a statistical analysis combining longitudinal studies of PSA.1 The researchers reported that all prostate cancer patients experience a change- point in the PSA growth rate, and normal patients do not experience a change-point at all. Using the PSA baseline growth rate for 20-year-old men for comparison, they found that the PSA value increases by an estimated 2.24% per year before the change-point; after the change-point, PSA increases by 15.31% per year for patients with localized prostate cancer and by 63.09% per year for patients with advanced metastatic disease. Most prostate cancer patients experience a transition at levels
of PSA lower than the frequently suggested 4.0 ng/mL clinical threshold (4.0 ng/mL) for considering an MRI scan or prostate biopsy.
The left panel of graph below shows that the predicted age at the transition is less than 60 years in nearly half of prostate cancer patients. The panel on the right compares the PSA growth curve in patients with localized and metastatic prostate cancer.
The median PSA for different age groups is 0.7ng/mL for men in their 40s, 0.9 in their 50s, 1.3 in their 60s, 1.7 in their 70s, and 2.1 in their 80s. Men whose PSA is higher than the median for their age group have a higher risk of having prostate cancer, clinically significant disease, and/or with 20 to 30 years of follow-up, metastases or prostate cancer-specific death.2-5 A PSA above the median of his age group for a man in his 40s is a stronger risk factor than his age, race, or family history.
This finding has clear implications for determining prognosis among newly diagnosed cases, suggesting that patients with high PSA are more likely to have aggressive disease than those with slowly increasing PSA levels and thus are candidates for aggressive therapy.
Dr. Catalona endorses the concept of the PSA velocity risk count, which counts the number of consecutive years in which a man’s PSA level rises by more than 0.4 ng/mL.6,7 For instance, a risk count of 2 indicates PSA increases exceeding 0.4 ng/mL in two successive years. His studies have shown that a PSAV risk count of 2 is associated with an 8-fold increase in prostate cancer risk and a 5-fold increase in the risk of high-grade disease. This approach aims to identify aggressive cancers earlier while potentially reducing unnecessary biopsies and overtreatment of non-life- threatening cases. Dr. Catalona uses the Prostate Health Index test for PSA testing, which measures 3 different PSA forms, the total PSA, percent-free PSA, and the [-2]pro-PSA8 (see separate QUEST article on page 6)
1. Inoue LY et al Biostatistics; 2004:5:483-500
2. D’Amico, AV et al N Engl J Med. 2004;351:125-35
3. Vickers AJ et al. BMJ. 2013; 346: f2023
4. Preston MA et al J Clin Oncol 2016; 34:2705-2711
5. Loeb S et al J Urol 177:1745, 2007
6. Carter HB et al Urology; 2007; 70:685-90
7. Loeb S et al BJU Int 2012; 109:508-13
8. Catalona WJ J Urol 2011; 185:1650-55