July 07, 2022
In the past, even patients with low-risk
prostate cancer would often be treated with surgery or radiotherapy, despite potentially serious side effects from the treatment. Recent years have seen a marked move away from immediate treatment of patients with low-risk prostate cancer. About
60% of patients with
low-risk prostate cancer now forgo treatment, opting instead for a regime of active surveillance (AS). However, some researchers, backed by pharmaceutical companies, appear to be exploring a new treatment approach for these patients. Dr. Catalona and other experts are quoted in this newly released article.
January 01, 2021
Gleason 3+3=6 is the lowest grade cancer in the traditional Gleason scoring system. Now, some urologists see a Gleason 6 as a noncancerous growth that has the potential to be invasive, but most likely will never spread to other organs or end up killing a man. Dr. Catalona opposes reclassifying Gleason 3+3 as noncancerous. “If somebody has an elevated PSA and gets a biopsy that shows one or two cores of Gleason 3+3 prostate cancer, it’s really not correct to tell them that they don’t have cancer and that they don’t require enhanced surveillance,” he said. He added that because of the well-recognized risk of biopsy sampling error, “All men with Gleason 3+3 are at substantial risk of their disease being underestimated.”
June 06, 2020
At the 2020 American Urological Association (AUA) conference, Dr. Catalona participated in a plenary session at the conference entitled Crossfire: Controversies in Urology: Prostate Cancer Active Surveillance Can be Done with mpMRI and Biomarkers; Biopsies are No Longer Necessary. The debate centered on the question of whether patients with low-risk disease on active surveillance still need a biopsy every two years, or whether the use of non-invasive biomarker tests or a multiparametric MRI can determine if they can skip these standard surveillance biopsies.
February 02, 2020
Dutch and American investigators published a modeling study that concluded lengthening the interval between prostate cancer screenings beyond two years for men with low PSA levels would reduce testing burden and overdiagnosis, although this would eventually lead to an increase in mortality. Dr. Catalona responded to the study for MedPage Today: “In my practice, I now see daily the sad effects of men who have had a hiatus in their PSA testing or have not been tested because their doctors have told them that PSA testing caused more harm than good. I believe that the message of this paper suggesting that less PSA testing is desirable could compromise many men.”
January 01, 2020
Chicago magazine named Dr. Catalona as a 2020 Top Doctor in Urology. The physicians on the list were chosen by their peers as the finest in the Chicago area.
December 12, 2019
In 2001, Syracuse University basketball coach Jim Boeheim was diagnosed with prostate cancer at age 56. Shortly after his diagnosis, Dr. Catalona performed Boeheim’s radical prostatectomy. Boeheim spoke to The Athletic about his diagnosis, treatment with Dr. Catalona and the work he’s doing to promote prostate cancer awareness, which includes speaking out about his disease, and reaching out to people facing and dealing with cancer. “The single most important message I can give is the importance of early treatment on certain cancers,” Boeheim told The Athletic. He recounted his battle with prostate cancer and how early screening saves lives. “It’s so important that I think every man needs to get tested at age 50. If you have a family history, you should be tested at 40. My kids? They’ll be tested at 35,” he said in the article.
December 12, 2018
Visual registration, in which multiparametric MRI targets are translated onto real-time ultrasound images, combined with image fusion software may offer the highest detection rate of clinically significantly prostate cancer and thus could aid in risk stratification, according to a new study published in European Urology. Dr. Catalona commented to Renal & Urology News, “Cost is a big issue in the US, where MRI scans are far more expensive, and many insurance companies do not cover them unless the patient has had a prior negative biopsy but still has a rising PSA.”
December 12, 2018
- Northwestern University Feinberg News Center
Men with inflammatory bowel disease have four to five times higher risk of being diagnosed with prostate cancer, reports a 20-year study from Northwestern Medicine published in the journal European Urology. Dr. Catalona is a co-author of the study.
November 11, 2018
- Northwestern Medicine Magazine
Moving from bench to bedside in just five years may sound like a daunting task, but the Lurie Cancer Center’s
Prostate Cancer SPORE is on track to produce tangible benefits for patients as it enters its fourth year, according to principal investigator William Catalona, PhD, professor of Urology.
September 09, 2018
A new European genomic study found that the prostate-specific ANO7 gene may play a critical role in the development of aggressive prostate cancer. The researchers found that tumors with certain genetic mutations in the ANO7 gene, as well as tumors that highly expressed the gene, led to worse prognoses for patients. Identifying genetic mutations such as this could lead to more accurate diagnostic tests. “This excellent study performed by a highly-respected, experienced research team has identified a relatively rare genetic variant that could be inexpensively genotyped as part of a biomarker panel that, along with other parameters, could help distinguish men with aggressive prostate cancer,” Dr. Catalona said in Cancer Network.
September 09, 2018
Castration-resistant prostate cancer (CRPC) occurs when patients develop resistance to androgen-deprivation therapy (ADT), also called hormonal therapy. A new study reported that certain prostate cancer cells that lack androgen receptors will not respond to current ADT treatments, and thus these cells contribute to the progression of cancer and development of CRPC. The study identified a potential new genetic pathway to target with drug treatment to stop the development of CRPC. Dr. Catalona noted that the researchers have translated their science to the clinic with a clinical trial of a drug previously FDA-approved to treat leukemia patients. “This landmark study may have a high impact and alter patient management,” Dr. Catalona told Renal & Urology News.
July 07, 2018
Aggressive therapy with curative intent appears to be highly successful in men with prostate cancer and Gleason score 10, according to a study published in the International Journal of Radiation, Oncology, Biology, Physics. In Renal & Urology News, Dr. Catalona commented, “It is questionable to what extent valid conclusions can be drawn from this study, especially concluding that radiation therapy plus hormonal therapy is more effective than surgery for Gleason 10 prostate cancer. The differences observed may be due merely to biases for which a complete adjustment is not possible by propensity-based analysis.
June 06, 2018
While some doctors say robotic prostate surgery leads to less blood loss and faster recoveries, other doctors say traditional open surgery remains the gold standard. The Wall Street Journal asked two experts to debate the topic. Dr. Ashutosh Tewari argued in favor of robotic surgery, and Dr. William Catalona presented his case in favor of traditional open radical prostatectomy. Dr. Catalona wrote, “For men choosing prostate surgery, a key decision is whether it should be performed with robotic assistance or by the traditional open method. Largely because of aggressive marketing, most prostatectomies are performed robotically. But it isn’t the best choice. There is no quality evidence that robotic procedures deliver better outcomes than open ones. Simply put, robotic prostatectomy advocates rely on studies with poor methodologies.”
March 03, 2018
Medscape’s coverage of the CAP Trial (see pages 1-2 of the Spring 2018 Quest) included extensive comments from Dr. Catalona. The largest-ever prostate cancer screening trial, in which asymptomatic men received a “one-off” blood test for prostate-specific antigen (PSA), has found no mortality benefit after 10 years. Dr. Catalona, an outspoken supporter of PSA screening, opined that the study design of CAP is unrealistic.
January 01, 2018
Dr. Catalona was named as one of Chicago’s top doctors in the urology specialty. Only 10 urologists received the recognition.
September 09, 2017
- Australian Financial Review
In an interview with the Australian Financial Review, Dr. Catalona explained his views on PSA testing and active surveillance. Dr. Catalona has “no doubt” about PSA”s importance as a screening tool for prostate cancer. Dr. Catalona said, “A man should be tested in his 40s and early 50s. At this age, his PSA should be less than 1. If it’s higher, then that is [the] most powerful predictor of the probability of him developing metastatic or lethal prostate cancer later in life. If it’s higher than 1 he should have more intensive screening going forward.”
May 05, 2017
- Northwestern University Feinberg News Center
Younger men with prostate cancer had a decreased risk of cancer progression while under active surveillance, compared to men older than 60, according to a study published in the Journal of Clinical Oncology. Dr. Catalona was a co-author of the paper. “This is a preliminary and somewhat paradoxical finding,” Dr. Catalona said. “Generally, active surveillance has been recommended only for men over the age of 65, because their shorter life expectancy would be expected to provide less time for prostate cancer progression to cause suffering or death. However, since prostate cancer behaves more aggressively in older men, they experience early cancer progression more frequently. A caveat concerning the early results of this study — with only a median of four years of follow-up — is that longer-term follow-up may reveal higher cancer progression rates in younger men.”
May 05, 2017
The debate on screening continues. Of the USPSTF’s 2012 recommendation against routine PSA screening, Dr. Catalona said, “We’re now seeing many more men come in with advanced, incurable disease – we’re undoing the good that was done over the past 25 years.” Dr. Catalona believes healthy men should have a baseline PSA blood test for risk stratification.
April 04, 2017
The U.S. Preventive Services Task Force (USPSTF) released an updated recommendation supporting individualized decision-making for PSA-based prostate cancer screening among men ages 55 to 69. MedPage Today spoke with leading experts in the field, many of whom see the USPSTF update as a tool to help them deliver better care to patients. “The new recommendation will now compel PCPs to at least discuss PSA screening with their patients,” Dr. Catalona said.
April 04, 2017
- National Public Radio, Morning Edition
In proposed revised guidelines, the U.S. Preventive Services Task Force says men ages 55 to 69 should decide individually with their doctors whether and when to undergo PSA testing. “PSA screening saves lives. I view it as a victory for PSA screening for prostate cancer,” Dr. Catalona said.
January 01, 2017
A study found that men whose lowest PSA score after radiation therapy for localized prostate cancer was greater than 0.5 ng/mL had an increased risk of dying before treatment failure. “There is a genuine need for surrogate endpoints for all-cause mortality in men with localized, unfavorable-risk prostate cancer, because it often takes 10 to 20 years for men to die after unsuccessful treatment for clinically localized disease,” Dr. Catalona told MedPage Today. He congratulated the authors for a good study involving an unmet need in prostate cancer.
July 07, 2016
The News Tribune featured Jerry Duttlinger, one of Dr. Catalona’s patients, in a series celebrating longtime cancer survivors in the Illinois Valley. Duttlinger’s experience “underscored another point he tries to impress upon people: Find a doctor and medical team you trust. To survive means to stay positive and for that you either must have complete faith in your providers or keep looking,” wrote the
News Tribune. Also, Duttlinger offers one firm piece of advice: “If you’re 40 or over, get the PSA test every year. Period.” You can view a video of Duttlinger talking about his experience with prostate cancer on the News Tribune website:
www.newstrib.com.
May 05, 2016
In recent years, major research organizations have begun to recommend active surveillance. Data shows that 40-50% of patients diagnosed with early-stage prostate cancer are choosing active surveillance, up from 10- 15% several years ago. However, it is not clear that everyone with a cancer scored as Gleason 6 or lower is a candidate for active surveillance. Dr. Catalona told the New York Times that he worried some younger men may find out too late that their cancer was worse than shown on the biopsy and has become incurable by the time they receive definitive treatment. Active surveillance, he warned, “is a tragic mistake for some.”
April 04, 2016
African-American men are approximately 70% more likely than Caucasians to develop prostate cancer. They are also 137% more likely to die because of a more aggressive form of the malignancy. Dr. Catalona told the Telegram that early detection holds the most promise to save the lives of African- American men and men of African descent. In 2012, the US Preventive Services Task Force advised against PSA screening. “It (the task force) recommended against all prostate cancer screening until you have symptoms,” said Dr. Catalona. “By the time you have symptoms from prostate cancer, it’s usually too far along to cure.”
December 12, 2015
According to preliminary data, fewer errors in PSA values than initially feared have turned up in a study of the National Cancer Institute (NCI) Surveillance, Epidemiology, and End Results (SEER) registrations. “From what I can discern from the analysis of the SEER data errors, the percentage of erroneous entries is relatively modest, and the possible effects on the results of some studies would seem to be small,” Dr. Catalona told MedPage Today.
December 12, 2015
- Northwestern Medicine Magazine
Northwestern Medicine scientists have received a five-year, $11 million grant from the National Institutes of Health National Cancer Institute (NCI) to lead a Specialized Program of Research Excellence (SPORE) in prostate cancer. The SPORE comes with demanding requirements, notably completing four studies that span the full translational research spectrum during the funding period. “The whole philosophy of a SPORE grant is that you have to take basic science from the research bench and move it to the patient’s bedside in five years,” said Dr. Catalona, principal investigator of the program. “Many projects could never qualify because you won’t see results in such an accelerated timeline. We’re driven to apply this research to help patients as soon as we can.”
November 11, 2015
Many urologists warned that the U.S. Preventive Services Task Force’s 2012 recommendation against widespread screening for prostate cancer would likely result in unnecessary deaths. Recent studies confirm that the testing and diagnosis of prostate cancer have dropped dramatically – likely the result of the task force’s flawed recommendation. Dr. Catalona predicted when the task force made its recommendation it could cause the prostate death rate to double by 2025. New research numbers suggest that more people, including those with aggressive forms of cancer, are forgoing screening and losing the opportunity for care.
October 10, 2015
In 1991, Dr. Catalona and colleagues published a report in the New England Journal of Medicine describing the use of PSA as a screening test for prostate cancer. “I think it’s easy to say that healthcare in men has not been the same since,” wrote David Graham, MD, author of the article.
September 09, 2015
Active surveillance – in which prostate cancer is regularly monitored for signs of progression – spares men whose tumors may never progress from potential treatment-associated adverse effects, such as sexual dysfunction or incontinence. Still, some clinicians remain skeptical about this approach. Dr. Catalona told HemOnc Today that the biggest problem with active surveillance is the frequency with which patients need to undergo biopsies to monitor their disease. The procedures can be painful and expensive, and some lead to sepsis or other adverse effects. “After biopsies, patients can get scarring around their prostate, and if they are found to need a nerve-sparing prostatectomy, it can be a lot more difficult because they had several biopsies,” Dr. Catalona said. “The other major problem is, 40% of men who fulfill the criteria for active surveillance and undergo radical prostatectomy have higher Gleason-grade cancer in their prostate or have cancer that has spread to the margins of the prostate or beyond,” Catalona said. “These patients who seem to be good candidates for active surveillance really are not. In studies that have good long-term follow-up, only about half of patients who enrolled in active surveillance but later had to undergo radiation or surgery had curable disease.”
July 07, 2015
Dr. Catalona was selected to be part of the Newsweek “Top Cancer Doctors 2015” list. The list was compiled through peer nominations and extensive research by Castle Connolly Medical LTD.
March 03, 2015
- Scientific American Prostate Disorders Bulletin
Since a (PSA) test isn’t enough on its own to differentiate prostate cancer from a prostate infection or benign enlargement of the prostate, doctors will typically advise men with PSA levels in the 4 ng/mL to 10 ng/mL range to undergo biopsy. This often results in a biopsy that is negative for prostate cancer. “In the past two years, this ‘one-size-fits-all’ approach to screening for prostate cancer has been modified thanks to the introduction of a more personalized, noninvasive risk assessment tool called the prostate health index, or phi,” Dr. Catalona wrote.
February 02, 2015
With cold and flu season in full swing, experts are warning men who have an enlarged prostate to avoid medicines containing antihistamines and decongestants. Nearly 80% of men age 50 and older will be diagnosed with some degree of the disease, said Dr. Catalona. “We don’t know what causes benign prostatic enlargement, it’s one of the great mysteries, and we really wish we did because it’s such a prevalent condition,” Dr. Catalona told Reuters Health.
November 11, 2014
Bleeding Orange is Jim Boeheim’s autobiography with Jack McCallum. Both the book and Jack McCallum’s online series about writing the book mention Dr. Catalona as Boeheim’s doctor. “We are both advocates for being PSA-tested, and we do what we can to talk about prostate cancer when asked about it,” McCallum wrote on his blog.
September 09, 2014
Dr. Catalona’s presentation at the 2014 AUA meeting in Orlando, Florida, was published in the AUA News as a “Crossfire Debate” with Dr. H. Ballentine Carter. Dr. Catalona wrote, “It has now been 1 year since the AUA membership was first stunned by the 2013 AUA guidelines, which are based on incomplete and flaws data, and inaccurate estimates of the benefits and harms of PSA screening.” See page 6 of the Winter 2014 QUEST for an adaptation of the presentation.
April 04, 2014
The Prostate Health Index (PHI) test is now available nationwide. Dr. Catalona said, “The problem is that higher levels of PSA can also be caused by benign enlargement or inflammation of the prostate, leading to many false- positives for cancer and ultimately unnecessarily invasive biopsies and an increased potential for patient harm.” The increase in accuracy of the PHI test addresses this concern.
March 03, 2014
- WBBM Newsradio 780 and 105.9
WBBM Newsradio highlighted the Winter 2014 issue of QUEST. Dr. Barry Kaufman said, “The Urological Research Foundation’s newsletter QUEST reports on recommendations from international groups, which it hopes will encourage men and their doctors to decide together what’s best for each patient.”
March 03, 2014
- International HIFU Blog
The clinical community is not fully on board with the U.S. Preventive Services Task Force (USPSTF) guidelines. Experts such as Dr. Patrick Walsh and Dr. William Catalona have taken issue with the panel’s decision regarding the PSA test.
March 03, 2014
According to a population-based study of Swedish men, blood PSA level at age 60 can differentiate men who benefit from prostate cancer screening and those who don’t. Dr. Catalona said, “In my opinion, it is a large leap of faith to recommend stopping PSA testing at age 60 based on the meager available data, especially since prostate cancer is a major cause of suffering and death, disproportionately higher in older men, and a PSA blood test is such a simple thing to do.”
March 03, 2014
The Economist cited Dr. Catalona as an advocate of the PSA test in its review of The Great Prostate Hoax by Richard Ablin and Ronald Piana. The review mentioned the studies that helped convince an American government panel to recommend that no man be screened for his PSA levels. “Critics such as Dr. Catalona said the trials were flawed,” said the article.
March 03, 2014
Northwestern Medicine, under the direction of Dr. William Catalona, was one of two health care providers to offer a new non-invasive blood test for prostate cancer. This new test, known as the Prostate Health Index (PHI), is three times as accurate as the standard PSA test.
February 02, 2014
WGN highlighted the PHI test as a new option for prostate cancer detection. “We looked at how many men would need to have biopsies if we just used the PSA test or if we used the PHI test. It turns out it saves about 30% of the unnecessary biopsies,” said Dr. Catalona.
February 02, 2014
Researchers are exploring whether multianalyte panels may be useful in detecting prostate cancer. In a webinar offered by the American Association for Clinical Chemistry (AACC), Dr. Catalona will describe results from the latest and most pertinent studies related to improving the process of prostate cancer detection.
October 10, 2013
MedPage Today asked a number of PCPs and oncologists if ordering a PSA test for men over 75 was clinically justified. “The truth is that the methodology used by the U.S. Preventive Services Task Force and other organizations for assessing the benefits and harms of PSA testing are biased in that they are bound to underestimate the benefits and overestimate the harms,” Dr. Catalona said.
June 06, 2013
The AUA guidelines are a step in the wrong direction for patient-centered care and may deprive many men of the opportunity to pursue shared decision making about possibly life-saving prostate-specific antigen (PSA) testing,” wrote Dr. Catalona in his commentary.
June 06, 2013
Dr. Catalona and his colleagues at Northwestern University completed a study on a new screening test for prostate cancer called the prostate health index, which is based on a new form of PSA called the pro-PSA. “It’s significantly more accurate than the PSA test and has a tendency to identify the more life-threatening prostate cancer,” Dr. Catalona said.
May 05, 2013
A pilot study showed that prostate-specific antigen peptidase activity is higher in patients with less-aggressive prostate cancer than in patients with advanced disease. At the annual AUA meeting, Dr. Catalona said this marker “may improve identification of men who may be better candidates for active surveillance” if confirmed by a larger study.
May 05, 2013
Dr. Catalona received the Society for Basic Urologic Research 2013 Distinguished Service Award for dedication and contributions to the field of basic urologic research
April 04, 2013
- Northwestern University Feinberg News Center
With the help of genetics, prostate specific antigen (PSA) screenings may become more accurate and reduce the number of unnecessary prostate biopsies, according to a new study from Northwestern Medicine. “If our results are validated, genetic adjustments could potentially prevent 15 to 20 percent of prostate biopsies,” said Dr. Catalona, senior author of the study. “Since it has been estimated that more than 1 million biopsies are performed in the United States annually, this could translate into 150,000 to 200,000 potentially unnecessary biopsies every year.”
April 04, 2013
A team led by Andrew Vickers, PhD, from the Memorial Sloan-Kettering Cancer Center in New York City proposes that just 3 PSA tests over the course of a lifetime is sufficient for many men. Experts say the study is not yet ready for clinical use. “It would be unwise to base any recommendation on such a small, single, unvalidated study, in my opinion,” Dr. Catalona commented.
March 03, 2013
New prostate cancer tests are coming to the market. “This field is moving kind of like cellphones,” Dr. Catalona said.
March 03, 2013
A collaborative research effort published in Nature Genetics verifies the benefits of whole genome sequencing in identifying genes associated with susceptibility to prostate cancer. Dr. Catalona said, “The hope is that this research could provide potential new targets for pharmaceutical manipulation in the treatment or prevention of prostate cancer in general.”
February 02, 2013
- Medill Reports – Chicago
A new study examined the link between fried food and prostate cancer. Dr. Catalona said, “You can’t do much about the genetics you inherit from your parents, but it’s widely acknowledged that your risk for cancer is a mixture of your genetics and your environment and how they interact with each other.”
February 02, 2012
- Northwestern University Feinberg News Center
Dr. Catalona is senior author of a new study that shows prostate-specific antigen velocity (PSAV) risk count testing may provide a more effective way for physicians to screen men for clinically significant prostate cancer. The new study, published by the British Journal of Urology International, shows the benefits of tracking a man’s PSA levels over time to help doctors more accurately assess his risk of life-threatening prostate cancer. “A persistently rising PSA is a harbinger for life-threatening prostate cancer,” said Dr. Catalona. “Our study findings show looking at how much PSA changes over time helps distinguish which cancers are aggressive more so than a single PSA value.”
May 05, 2011
- Northwestern University Feinberg News Center
A man’s rising PSA (prostate-specific antigen) level over several years, which has been seen as a possible warning sign of prostate cancer, has recently come under fire as a screening test because it sometimes prompts biopsies that turn out to be normal. A new study, however, shows nearly 70 percent of men who had rising PSA levels and subsequent normal biopsies were eventually diagnosed with prostate cancer, according to research from Northwestern University Feinberg School of Medicine. The trend of a PSA level over several years is called PSA velocity. Dr. Catalona is lead investigator of the study. “Our findings show an elevated and rising PSA level or velocity should lead a clinician to follow a patient more closely, even if he has a negative biopsy,” he said. “One negative biopsy isn’t the end of the road.”
April 04, 2011
- Northwestern University Feinberg News Center
In a large, multi-center clinical trial, a new PSA test to screen for prostate cancer more accurately identified men with prostate cancer – particularly the aggressive form of the disease – and substantially reduced false positives compared to the two currently available commercial PSA tests, according to newly published research from Northwestern Medicine. “This new test is more specific and accurate than the currently available blood tests for early prostate cancer detection,” said lead investigator William Catalona, M.D. “This will focus on the detection of more life-threatening prostate cancers and reduce unnecessary biopsies in men 50 years of age and older.”
November 11, 2010
- Northwestern University Feinberg News Center
The Alpha Omega Alpha (AOA) medical honor society recently welcomed its newest members at a ceremony hosted by Northwestern University Feinberg School of Medicine. Inductees included medical students, residents, and faculty members, as well as an alumna — each selected based on their academic performance or contributions to the medical field. Dr. Catalona was inducted as a faculty member.
June 06, 2010
- Northwestern University Feinberg News Center
New research from Northwestern University Feinberg School of Medicine and the University International Institute for Nanotechnology shows that an ultrasensitive PSA test using nanoparticle-based technology may be able to definitively predict after surgery if the cancer is cured long term or if it will recur. “These studies suggest that the nanotechnology PSA test might become the preferred postoperative PSA test for men who have been treated with radical prostatectomy,” said Dr. Catalona, a senior investigator on the study. “It should be especially useful in the early identification of men who would benefit from adjuvant postoperative radiation therapy and those who need postoperative salvage radiation therapy for recurrence.”
August 08, 2009
PSA testing is a prominent example of how a “normal” clinical value is derived, accepted, and continuously revised.
April 04, 2009
- William J. Catalona, MD
The use of ciprofloxacin (Cipro) as a test to see whether an elevated PSA level will decrease is controversial. His current practice is to prescribe an antibiotic other than Cipro to see if the PSA decreases.
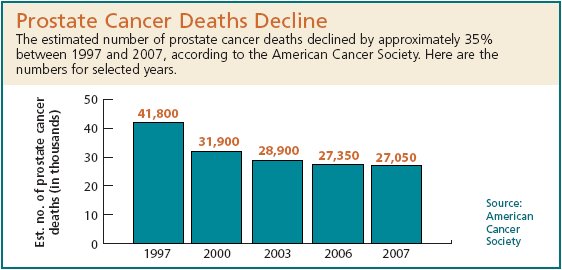
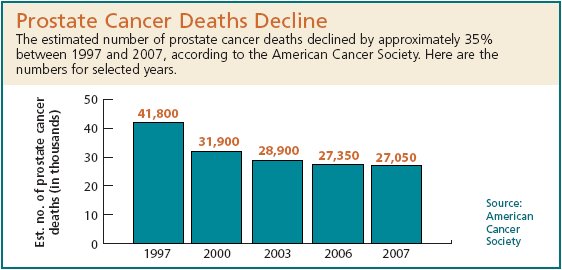
April 04, 2009
- American Cancer Society
More than 90% of all prostate cancers are discovered in the local and regional stages; the 5-year relative survival rate for patients whose tumors are diagnosed at these stages approaches 100%. According to the most recent data, relative 10-year survival is 93% and 15- year survival is 77%. The dramatic improvements in survival, particularly at 5 years, are partly attributable to earlier diagnosis and improvement in treatment. Modern methods of detection and treatment mean that prostate cancers are now found earlier and treated amore effectively. If a man is diagnosed this year, his outlook is likely to be better than the numbers reported above. Modern methods of finding and treating prostate cancer have led to a yearly drop in death rate from prostate cancer. Men treated today may have an even better outlook than the numbers above.
April 04, 2009
- William J. Catalona, MD
Two PSA test standards are causing serious problems for early detection of prostate cancer. If patients and their doctors are not aware of the differences in tests, early diagnosis and life-saving treatment could be delayed. The issue involves how PSA test results are reported and interpreted.
August 08, 2008
- by William J. Catalona, MD
I am not a fan of active monitoring or watchful waiting in what are being called low-risk prostate cancer (CaP) patients.
August 08, 2008
This article reports on a study that addresses the question: Do the 3 significant 8q24 prostate cancer susceptibility regions predict aggressive disease?
July 07, 2008
This article continues our coverage on new discoveries in the genetics of prostate cancer that continue to change the way researchers view the development of prostate cancer and on the important contributions of Dr. William Catalona and his collaborators.
August 08, 2007
- by William J. Catalona, MD
Recent studies have provided new information and new practices for the use of Hormonal Therapy in the treatment of prostate cancer. Dr. Catalona updates his previous writing on this topic.
August 08, 2007
- - by Cecilia Lacks, PhD
A new model for studying the genetics of cancer is replacing the traditional perspective f studying one gene carried through generations of a family. Now, researchers are looking at several risk alleles and studying how they interact with each other.
December 12, 2006
- This information is an adapted version of a medical journal article written by William J. Catalona, MD; Misop Han, MD; and Stacy Loeb, MD
Should Screening for Prostate Cancer Begin Before 50? Should a PSA Below 4 Trigger a Biopsy? Should Men 70-75 Be Screened for Prostate Cancer?
May 05, 2006
This OpEd Piece in the Washington Times by Dr. Richard Atkins, CEO of the National Prostate Cancer Coalition, explains whey the PSA Test is so important in detecting prostate cancer early enough to save lives. He says we can’t “attack the PSA test while research attempts to discover a better one. It’s the only test we have.”
April 04, 2006
At a recent Prostate Cancer Symposium, Dr. Catalona presented the argument that the benefits of universal PSA screening for prostate cancer outweigh the risks. This article summarizes his views and the research supporting them. Also, he pointed out that he recognizes the medical community is polarized with regard to prostate cancer screening. Epidemiologists and primary care physicians can be skeptical about the value of universal PSA screening while urologists and radiation and medical oncologists tend to see its benefits.
April 04, 2006
- Essential Science Indicators
Dr. Catalona’s studies and reports on prostate cancer research are among the most high cited in other scientists’ and doctors’ papers and findings. For that reason, Essential Science Indicators, an organization that analyzes medical research, asked to interview him about his high-cited prostate cancer research. This interview discusses his research and also explains how and why he became a prostate cancer surgeon and resesearcher.
April 04, 2006
This article in Business Week discusses the topic of for-profit treatment centers competing with community and teaching hospitals in the treatment of cancer patients. But it points out that for many people, particularly those with rare forms of cancer, the medical-school centers remain the preferred option. The article refers to the work of Dr. Catalona saying, “Although there are no national data ranking cancer facilities by survival or recurrence rates, studies have shown that patients do better when their surgeons have performed the same operations over and over again. For example, Dr. William J. Catalona, director of Northwestern’s clinical prostate-cancer program, has performed 4,700 nerve-sparing prostate removals, and is still doing 25 to 30 a month.”
June 06, 2005
Three patients of Dr. Catalona’s have joined forces to get their message out to everybody: “Get tested.” Dr. Catalona concurs with this and explains that waiting can be too late if the cancer has moved from a curable stage to an incurable stage.
April 04, 2005
A HealthDay.com article talks of a recent study that statins, taken for lowering cholesterol, may also lower the risk of advanced prostate cancer. Dr. Catalona and colleagues were interviewed for their views on this study.
May 05, 2004
An article in USA Today announces that a national network of cancer centers is recommending a much more aggressive approach to prostate cancer screening.
March 03, 2004
Dr. Catalona, co-author of a new study on lowering PSA threshold for biopsy to 2.5, was quoted in the Wall Street Journal (March 23, 2004), “To Improve Prostate-Cancer Detection, Doctors Change Approach to Testing.” In the article, Dr. Catalona said that for many men, lowering the threshold simply means they’ll get a biopsy sooner rather than later. In a 12-year, 36,000-man study in St. Louis, doctors charted rising PSA scores for a number of men who weren’t given a biopsy or diagnosed with cancer until their score finally hit 4. “These men would look at their PSA record and say, ‘The writing’s been on the wall for a long time. Why didn’t we do that biopsy earlier?”
November 11, 2003
This USA Today article uses the announcement of Robert De Niro being diagnosed with prostate cancer to introduce the idea of early detection through PSA screening and what that early detection has meant in terms of treating prostate cancer more effectively. Dr. Catalona is one of the medical sources for the article and is quoted saying, “PSA is the best and most accurate risk assessment test in all of medicine.”
November 11, 2003
A brief reference in Newsweek Magazine brings up some pros and cons of prostate cancer screening. Dr. Catalona is quoted in the piece as saying, “The only way to detect (prostate cancer) while it is curable is to be proactive. Get screened.”
September 09, 2003
“Could Your Husband Be At Risk”, in the September 2003 issue of Woman’s Day magazine is based on an interview with Dr. Catalona and is a brief summary of the key factors in the diagnosis and treatment of prostate cancer.
Dr. Catalona says in the article, “Women should encourage the men they love to get regular screenings. Prostate cancer develops silently and screenings are the only way to detect it.”
August 08, 2003
This Washington Post article reports on a clinical study finding published in the July 2003 New England Journal of Medicine which indicates the current cutoff of PSA 4 for recommending biopsies should be lowered in order to save more lives. Dr. Catalona is a co-author of the journal article and a research partner in the study. Blood samples from his 15 year PSA study were an integral part of the research for this finding. Since 1995, Dr. Catalona has been using a 2.5 PSA cutoff for recommending prostate biopsies.
July 07, 2003
Dr. Rinaa Punglia and her research team in Boston collaborated with Dr. Catalona to evaluate 6,691 volunteers from Dr. Catalona’s research studies in the area of PSA testing and prostate cancer diagnosis. This Wall Street Journal article reports on the study, published in the New England Journal of Medicine, which found that the results of the PSA blood test could be dramatically improved by simply lowering the threshold for what is considered a problematic result from 4.0 to 2.5. This article also includes the views of doctors who are not certain that earlier detection of prostate cancer is helpful in improving disease outcomes.
July 07, 2003
This website article on HealthDay.com reports on Dr. Catalona’s findings that a biopsy should be done when the PSA reading reaches 2.5. The article also includes the views of doctors with different perspectives.
April 04, 2003
Dr. Catalona and his research collaborators comment on their findings that genetics causes some men to test higher on the PSA blood test in this website article on amednews.com Dr. Catalona says, “We’re going to need better tests to identify more aggressive cancers.”
August 08, 2002
- American Association for Clinical Chemistry
Doctors have struggled for years with the limitations of diagnosing prostate cancer by measurement of PSA (prostate-specific antigen).
Although the highest levels of PSA (above 10ng/mL) are closely connected to the presence of prostate cancer, the middle and lower ranges are more difficult to interpret. Now, research results, coming from the study of Dr. Catalona’s patients, show that the time has come to lower the PSA test cutoff point for biopsy from 4.0 to 2.5. This article explains the study recommending the change and includes responses from doctors regarding the recommendation.
July 07, 2001
- Proact (Prostate Cancer Action Website)
Former baseball star and general manager of the Houston Astros and New York Yankees, Bob Watson talks about his experience with prostate cancer surgery by Dr. Catalona.
February 02, 2001
William J. Catalona, M.D., professor of surgery and director of the Division of Urologic Surgery, recently received the 1998 Eugene Fuller Triennial Prostate Award from the American Urological Association.
January 01, 2001
Dr. Catalona joined a live chat on ABCNEWS.com to discuss PSA testing and the latest treatment options for prostate cancer.