Reports From Dr. Catalona’s Follow-Up Studies
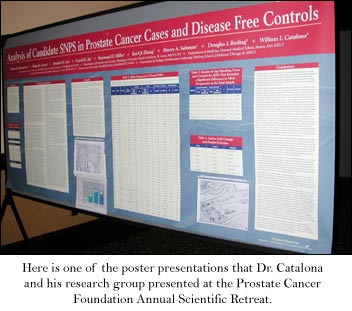
Dr. Catalona and his research collaborators delivered their research findings at the Prostate Cancer Foundation Annual Scientific Retreat and at the American urological Association (AUA) annual meeting.
Although the information is technical, the following summaries are written with QUEST readers in mind.
We would like you to be familiar with the direction of the research and the vocabulary associated with it.
Some of the information has practical applications now. Some shows the beginning of research projects with exploration or new understanding as the main purpose, and hopefully, practical applications will follow.
Surely, though, this research will define how prostate cancer is diagnosed, treated and hopefully prevented in generations to come.
Post-operative PSA Doubling Time (DT)
Doubling time is a significant indicator of the aggressiveness of the cancer. It is the time it takes the rising PSA to double itself.
Question: Could we use information at the time of a prostate cancer diagnosis to determine if a patient was at risk for recurrence and if the information could predict a patients potential life span?
We looked at the PSA level, Gleason score, and the clinical tumor category to see if they could predict post-operation PSA DT and overall mortality rates.
If we found a correlation between this pre-operation information and what would likely happen after surgery, then we would be able to recommend ost operative radiation treatment for those who would most likely need it, perhaps without waiting for a rising PSA.
At the same time, we could stop overtreatment for those who would most likely do fine without the radiation, even though they have a slightly rising PSA after surgery.
Conclusion: Our study found that if a pre-operation PSA Velocity (rise) is more than 2.0, then its likely a post-operation PSA doubling time will be less than three months.
This information suggests a high-grade disease and a shorter survival. Radiation therapy should be started as soon as possible.
Our study found that in men with a pre-operation PSA Velocity of 0.5 or less, a persistent PSA after surgery will more likely stay low, reflecting some residual benign prostate gland tissue or some non-active microscopic cancer. These men may not require radiation therapy.
Anthony V. DAmico, MD, PhD; Ming-Hui Chen, PhD; Kimberly A. Roehl, MPH; William J. Catalona, MD
Accuracy of Prostate Weight Estimation
The ability to estimate prostate weight is useful in many CaP treatment decisions.
Question: Is it more accurate to estimate prostate weight from a digital rectal exam (DRE) or a transrectal ultrasonography (TRUS)?
We looked at the accuracy of the two methods by comparing the weight estimates before a radical prostatectomy (RRP) to the actual weight of the gland following a RRP.
Conclusion: DRE estimates of prostate weight were not accurate. TRUS estimates correlated moderately well, especially for smaller glands. In general, though, a TRUS estimate was smaller than the actual weight of the gland.
Stacy Loeb, Misop Han, Chicago, IL; Kimberly A. Roehl, Jo Ann V. Antenor, St. Louis, MO; Xiaoying Yu, William J. Catalona
Predicting Future Prostate Cancer In men with PSA of 2.6-4 and Initial Negative Biopsy
Approximately 75% of men in our study with a PSA of 2.6-4 had no evidence of prostate cancer on biopsy. But within six years, 11% of those men were diagnosed with prostate cancer. Deciding whether and when to repeat the biopsy is challenging.
Question: What factors would be useful in identifying men in the above category who have an increased risk for being diagnosed with prostate cancer at a later time?
We looked at several factors involved in prostate cancer diagnosis: free and total PSA, age, family history, DRE, biopsy results, prostate volume, PSA density, and PSA velocity.
We found only two of them to be significant: biopsy results showing HGPIN and PSA Velocity.
Conclusion: Men with a PSA of 2.6-4 and a negative biopsy should be advised to have a repeat biopsy if they have HGPIN or a PSA velocity of 0.3 or more.
Scott E Eggener, Kimberly Roehl, Misop Han, William J Catalona
Connection of DRE Exam Findings to Cancer Aggressiveness
Since the introduction of PSA screening, the great majority of prostate cancers are diagnosed in patients who dont show physical symptoms in a digital rectal exam.We were interested in those who do.
Question: Is there a difference in the aggressiveness of the cancers felt in a DRE and those not felt?
Our study looked at 389 men who had a RRP with the same doctor. We compared information in those patients with a negative DRE and those with a positive one. (The cancer could be felt.)
We looked at pathology features that would tell us whether the cancer was organ confined or not. And we compared cancer volume in the two groups.
Conclusion: Men whose prostate cancer can be felt in a DRE have higher Gleason grades and a greater percentage of non-organ confined disease than those who dont.
Robert B. Nadler, Xiaoying Yu, Misop Han, Joseph Pazona, William J. Catalona
Treatment of Localized Prostate Cancer
It has been suggested that with long-term, widespread PSA screening and the use of biopsy, many prostate cancers detected and treated in the past five years are possibly harmless. We wanted to address that concern in this study.
Question: Does PSA testing detect curable, clinically significant cancer?
The established criteria for possibly harmless prostate cancers is when the cancer is less than 0.5 cubic centimeters, organ confined, and has a Gleason score of 6 or less. (While Dr. Catalona uses these criteria, he does not believe that anyone can say which cancers are truly harmless and which will in time change to high-grade, deadly cancers.)
Prostate cancer which rises about the levels in this criteria is considered clinically significant cancer, meaning if left untreated, it will most likely cause death.
This study looked at two groups of men with a PSA over 4 and two groups of men with a PSA over 10. Both groups of men had a RRP.
Using the criteria to determine clinically significant cancers, 99% of the patients in the group from one surgeon and 100% of the patients in the group from other surgeons had clinically significant cancers.
Conclusion: In the recent PSA era (2001-2004), the great majority of patients diagnosed and selected for treated with radical prostatectomy have potentially curable prostate cancer that has features associated with clinically significant tumors.
Misop Han, Xiaoying Yu, Norm D. Smith, Robert B. Nadler, William J. Catalona











