The Prostate Health Index (PHI) Blood Test

The goal of PSA screening is to test asymptomatic men and improve health outcomes by diagnosing the cancer at an early stage. A benefit of screening is to decrease the proportion of advanced-stage cases at the time of diagnosis and thus decrease suffering and death from prostate cancer, which is the second-leading cause of cancer death in US men. During the PSA screening era (1991-present), the US prostate cancer death rate has decreased by 52%. However, PSA screening has been controversial due to numerous limitations. Although higher PSA levels are a strong predictor of prostate cancer risk, the total PSA measurement is not specific for prostate cancer because other factors, such as benign prostatic hyperplasia, prostatitis, and other benign conditions, affect PSA levels. Consequently, many men undergo unnecessary biopsies, leading to the over-detection of some indolent tumors.
The Prostate Health Index (PHI), approved by the US Food and Drug Administration in 2012 (Dr. Catalona led the pivotal studies for FDA approval) for men whose total PSA levels are between 4 and 10 ng/mL (although studies have shown that it is also robust with PSA levels as low as 2.5 and above 20 ng/mL). The National Comprehensive Cancer Network guidelines for early prostate cancer detection suggest PHI as a supplementary biomarker for PSA testing. It addresses many of the drawbacks associated with PSA screening. Its specificity is greater because PHI combines three different circulating forms of PSA, total PSA, free PSA, and [−2]pro-PSA, in the mathematical formula.
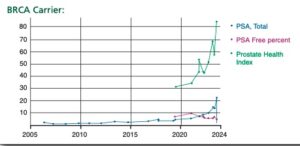
Dr. Catalona incorporates a PHI flow chart in the electronic medical record of his patients that displays the serial levels of the three PSA forms over time in different colors. In this display, the blue line charts the total PSA, which he would like to remain low and decrease after treatment. The red line represents the percentage of free PSA, which is an indicator of the extent to which any PSA in the blood is due to a benign condition, such as benign enlargement (BPH – benign prostatic hyperplasia), inflammation, recent sexual activity, or an intense bicycle ride. Dr. Catalona wants this level to be high (greater than 25% and not less than 10%), as it indicates that a high PSA level might not be due to prostate cancer. The green line is the most important, as it represents the PHI. Dr. Catalona wants this to be less
than 30, as it predicts that if the patient underwent a prostate biopsy that day, there would be only about a 10% chance or less that the biopsy would show prostate cancer.
Thus, PHI is a simple blood test, but it outperforms any of its individual components for identifying clinically significant prostate cancer. Increasing PHI scores predict a greater risk of high-risk pathology and biochemical recurrence after radical prostatectomy. PHI performed at the initiation and during active surveillance predicts subsequent tumor up-grading in surveillance biopsies.
Catalona WJ et al J Urol. 2011; 185:1650–1655