Early Diagnosis of Prostate Cancer Through PSA Testing Saves Lives


An accumulating body of increasingly compelling evidence shows that PSA screening can reduce prostate cancer (CaP) deaths and is changing the way clinicians view prostate cancer screening.
When you think about it, there would be no point in trying to detect prostate cancer early if there were no effective treatment for early-stage disease.
The study on the long-term results of a Swedish randomized trial of radical prostatectomy versus “watchful waiting” for early prostate cancer shows that surgery can reduce the rates of metastases and CaP deaths, and increase overall survival.
But the holy grail of screening is the randomized trial, so let’s look at the evidence from randomized trials on PSA screening.

Randomized Trials
In the initial report from the European Randomized Trial (ERSPC), men randomized to screening had 40% fewer advanced CaP cases at diagnosis and a 20% lower CaP death rate. Not surprisingly, the mortality benefit was observed largely in men under 70.
However, the initial report contained the sobering estimate that 48 men had to be treated to prevent 1 prostate cancer death. This high, and now widely-quoted, NNT (number needed to treat) of 48 raised many eyebrows, because it is shocking to think that 48 men would have to undergo surgery or radiation to prevent 1 man from dying of prostate cancer.
But because the risk of dying from prostate cancer is influenced by a patient’s life expectancy, the NNT to save 1 life is also strongly influenced by a patient’s age, his health and the length of follow-up of the trial.
The NNT is lower in younger, healthier men and in trials that have longer follow-up, much lower.
NNT Lower in Younger, Healthier Men
In the well publicized U.S. study, (PLCO), a less-well-known and far less-quoted follow-up analysis of PLCO data showed a striking lifesaving benefit in the roughly one-third of PLCO participants who, other than having prostate cancer, were basically healthy.
These screened patients in PLCO had a whopping 44% lower CaP death rate. And the NNT to save 1 life in these healthier men was reported to be 5.
Data Providing Support for Screening

The Norrköping Trial, from Sweden, is another trial that was widely publicized as being a “negative screening trial.”
But the data actually provides considerable support for PSA screening.
First, the screened patients had far fewer advanced tumors at diagnosis.
Second, there was a strong trend for better CaP-specific survival in the screening arm.
And third, there was a significantly lower risk ratio for prostate cancer death in the screening arm.
“Opponents of screening who suggest that men should not seek early prostate cancer diagnosis are doing a disservice to the public.”
Best Methodology
In my opinion, the screening trial with the best methodology is the one from Goteborg, Sweden.
Unlike either PLCO or the European Trial, the study population is younger and presumably healthier – 20,000 men aged 50-64.
The Goteborg trial participants were screened every 2 years with progressively lower PSA cutoffs over time beginning with a 3.4 cutoff and ending with 2.5.
Moreover, 93% of the men complied with the biopsy recommendation when they had an abnormal screening test, and a full 77% had 14 years of follow-up.
The results of this excellent trial show that 41% fewer screened patients were diagnosed with advanced disease, and they had a 44% lower prostate cancer death rate.
Moreover, in the Goteborg Trial, at 14 years of follow-up, the NNT was 12, a far cry from 48. This NNT compares favorably with the NNT for breast cancer, which is 10 at 10 years of follow-up.
Other Evidence
In addition to looking at the results from the trials, it is useful to examine the epidemiologic evidence (Epidemiology is the study of the health-event patterns in a society.) that PSA screening saves lives.
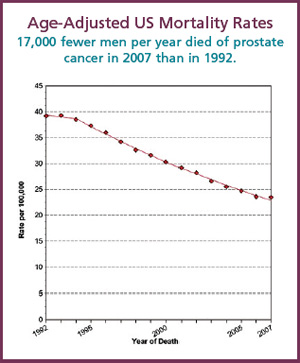
The National Cancer Institute SEER (Surveillance Epidemiology and End Results) database shows a 75% decrease in metastatic disease at diagnosis during the PSA era and a 40% decrease in the age-adjusted prostate cancer death rate.
Doing the math, in 1992 there were 131 million US males, and the age-adjusted CaP mortality rate was 39.2 per 100,000 males, which accounted for more than 51,000 CaP deaths.
By 2007, which is the most recent SEER data available, the US population had grown to 149 million men, but the age-adjusted CaP mortality rate had decreased from 39.2 to 23.5. This number amounts to about 35,000 fewer CaP deaths, meaning that 17,000 fewer men died of prostate cancer in 2007 than in 1992, the beginning of the PSA era.
But, does PSA screening really deserve credit for the decreasing prostate cancer death rate? Two mathematical modeling teams from the NCI’s (National Cancer Institute) modeling network independently projected what the CaP death rate would be in the absence and presence of PSA. They reported that 45 to 70% of the benefit could be attributed directly to PSA screening.

“Screening is necessary to give patients the full range of treatment options at the earliest possible time.”
Trends Outside US
Similar trends are reported in the WHO (World Health Organization) database in countries where PSA screening is widespread but not in those where screening is not practiced.
Declining trends in prostate cancer deaths during the PSA era took place in countries where PSA screening is practiced – US, Canada, France, Germany, and Spain.
In contrast CaP death rates continue to increase in countries where PSA screening has not been widely adopted – Belgium, Denmark, Greece, Ireland, Bulgaria.

In Austria, regular PSA testing was made available to residents of the state of Tyrol beginning in 1993 – but not elsewhere. Tyrol has a 54% reduction in CaP deaths during the PSA era versus 29% decrease in the rest of Austria. PSA screening is rare in Northern Ireland, with only about 6% of men screened. Comparing these Irish men to men in the screening arm of the European Randomized Trial, where 94% were screened, the European Screening Arm had a 53% lower rate of metastases at diagnosis and a 37% lower CaP death rate.
Disservice to Public
We have all witnessed the many anti-PSA screening articles in newspapers, magazines, medical journals, newscasts, and on the Internet. They have appeared in increasing numbers in recent years. And they are having the effect of discouraging many men from undergoing PSA screening.
In my practice, I have seen primary care physicians as patients who stopped monitoring their own PSA levels or ignored their own rising PSA levels for years, only to be diagnosed later with advanced disease.
In my opinion, the opponents of screening who suggest that men should not seek early prostate cancer diagnosis are doing a disservice to the public.
Screening is necessary to give patients the full range of treatment options at the earliest possible time.
The USPSTF (United States Preventive Services Task Force) is a US Government agency, and its panel is now reviewing its prostate screening recommendations. The previous panel included no urologist or medical oncologist. In 2008, they concluded that there was insufficient evidence to recommend for or against PSA screening in men under age 75, but that men over 75 should not be screened.
On the other hand, the AUA (American Urological Association) and the ACS (American Cancer Society) have adopted cautiously positive recommendations for prostate cancer screening, and the NCCN (National Comprehensive Cancer Network) have produced guidelines to help physicians implement screening in men who have decided they want to be screened.
However, with the USPSTF and the American College of Preventive Medicine claiming insufficient evidence for screening benefits, the medical community has become polarized, and patients and even their physicians have become confused.

Recommendation
Several current guidelines suggest that men with a 10-year life expectancy should have an informed discussion of the benefits and risks of PSA screening. If they decide to be screened, a baseline PSA and DRE (Digital Rectal Exam) should be performed at age 40 to assess their individual risk.
If the risk is high, as defined by having a strong family history of prostate cancer, being of African-American race, having a base-line PSA of more than 1, or a PSAV (PSA Velocity) of more than 0.35 ng/mL/year; then, annual screening is indicated.
If the risk is average, repeat screening is recommended at age 45 and then, if the individual risk still appears to be average, annual screening should begin at age 50.
Urologists should try to educate primary care physicians that PSA screening, performed wisely, will save lives — perhaps their own.
(ERSPC)











